
By Ishara Nanayakkara
In October, The Pew Charitable Trusts released an analysis of the core measures states can use to address and mitigate the opioid epidemic. The information included in this article originates from this analysis.
This article is the first in a three-part series. The second article can be viewed here.
Overview
The U.S. continues to experience an increasing number of deaths due to the opioid epidemic. There are significant gaps between the number of people that could use medication to treat opioid use disorder and those receiving medication. The Substance Abuse and Mental Health Services Administration 2021 National Survey on Drug Use and Health found that only 22% of people with an opioid use disorder received medication-assisted treatment for opioid misuse. The most effective drug treatments for opioid use disorder are methadone, buprenorphine and naltrexone.
- Methadone reduces craving and withdrawal symptoms and blunts the effects of opioids.
- Buprenorphine, like Methadone, diminishes cravings and withdrawal symptoms and increases safety in cases of overdose.
- Naltrexone blocks the euphoric and sedative effects of opioids and suppresses and reduces cravings.
To close this gap, states need a set of core metrics to track relevant data and provide a comprehensive picture of care for opioid use disorder. Many states have dashboards tracking overdose deaths, but only a few states track a full range of metrics including rate of diagnosis, FDA-approved medication distribution and number of treatment providers.
To address this issue, The Pew Charitable Trusts convened a panel of experts in September 2021 to identify treatment goals using the “cascade of care” method, which identifies key measurements in the life cycle of a chronic disease.
Pew’s expert panel applied the “cascade of care” framework and defined the stages as:
- Opioid use disorder identification/diagnosis: Having a formal diagnosis in a medical record or claim.
- Initiation of treatment: Receiving treatment services.
- Retention in opioid use disorder treatment: Staying engaged in treatment for at least six months.
- Recovery: Reaching a state defined by SAMHSA as “a process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential.”
The panel consisted of state and federal officials, treatment providers, experts in health measurement and analytics, advocates, and individuals with lived experiences. The panel agreed on several core measures for tracking opioid use disorder based on the stages of the cascade of care:
- Opioid use disorder identification/diagnosis
- Diagnosis: Percentage of people who had a documented diagnosis, including on an insurance claim.
- Percentage of people assessed using a standardized screening tool: Rate of assessment using tools such as the Drug Abuse Screening Test or the Tobacco, Alcohol, Prescription Medication, and Other Substance Use tool.
- Initiation of treatment
- Use of pharmacotherapy: Percentage of people diagnosed with an opioid use disorder who received medication.
- Opioid use disorder provider availability: Number of providers and treatment programs that can provide medication for opioid use disorder.
- Retention in opioid use disorder treatment
- Continuity of pharmacotherapy: Percentage of people receiving medication for opioid use disorder who used medication for at least six months.
- Initiation of and engagement in opioid use disorder treatment: Percentage of people who initiated treatment within two weeks of diagnosis or percentage of people using two or more services within the first month after initiating treatment.
- Follow-up after an emergency department visit for substance use: Percentage of people who receive follow-up care for substance use disorder or an overdose within seven days, and 30 days after visiting an emergency department for a substance use disorder related issue.
- Recovery
- One or more patient-reported outcome measures to be determined by state: Percentage of individuals who achieve an improved level of functioning or quality of life.
Note: Read The Pew Charitable Trusts’ issue brief, “States Should Measure Opioid Use Disorder Treatment to Improve Outcomes,” to read more about each measure and how it was selected.
The panel recommended states implement these core measures to provide stakeholders with information. Access to the data may improve practices and target scarce resources where they are urgently required and will be most effective. Pew also recommends that states develop public action plans including:
- Creating a data plan that includes reporting data publicly to create accountability.
- Regularly reviewing and acting on data.
- Working with treatment providers and people with opioid use disorder to develop improvement initiatives.
- Organizing data by demographics, such as race, age, and gender, to uncover health inequities.
Applying the Cascade of Care to Opioid Use Disorder
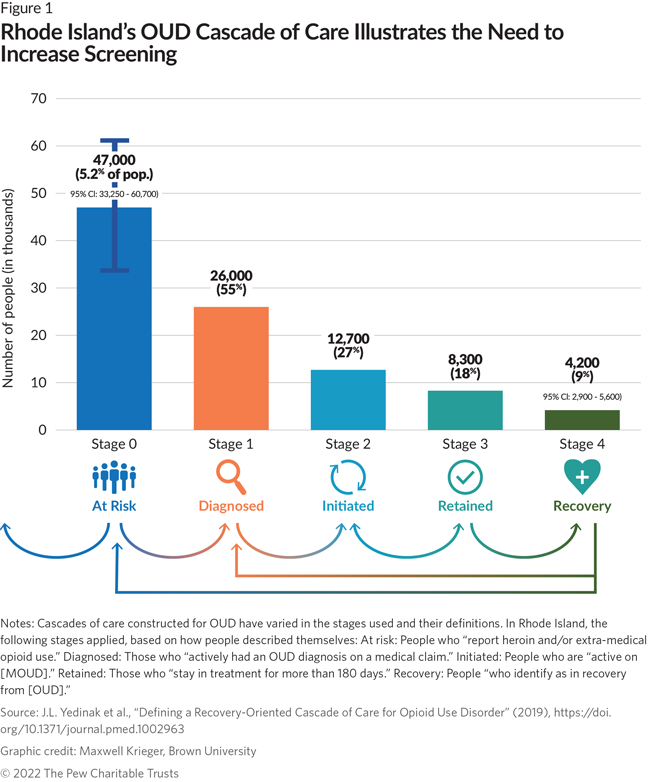
Applied globally, the “cascade of care” model improved the treatment of chronic diseases such as hepatitis C, hepatitis B, diabetes, and tuberculosis. Researchers funded by the National Institute on Drug Abuse recommended the “cascade of care” framework be applied to the opioid epidemic in 2017. Since then, several states, localities and Tribal nations using the method established metrics for specific programs. States can apply the cascade of care approach to see which aspects of their treatment system are effective and which require increased attention and resources. Using the cascade of care model, Rhode Island found a gap between the number of people at risk for opioid use disorder and the number of people screened. Based on these findings, state officials decided to focus on increasing screening efforts for at-risk citizens.
A Toolkit for Adopting Core Opioid Use Disorder Treatment Measures
To help policymakers and data analysts adopt the core metrics, Pew commissioned an implementation toolkit by Dr. Tami Mark, senior fellow at RTI International. This toolkit provides:
- A checklist of activities to implement and improve policies and programs.
- Detailed information about each metric, including the data used, the organization responsible for updating the information, and links to additional technical details.
- A description on how measures can be used to identify inequities in access and use of treatment by populations of interest.


